Dr. Ajay Anand
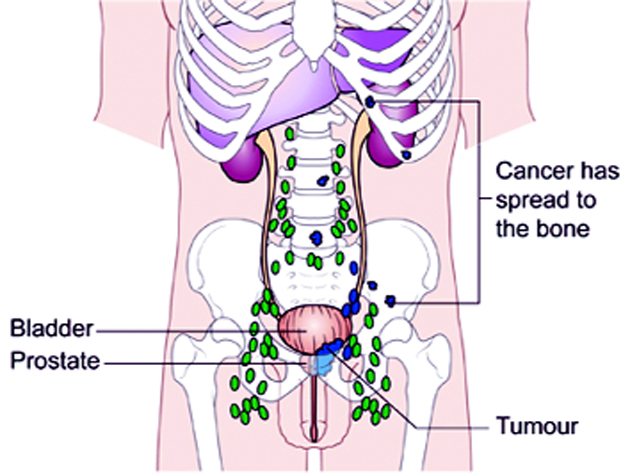
Locally Advanced Prostate Cancer is a clinical diagnosis whereby the tumour has extended beyond the prostatic capsule with no evidence of nodal or distant metastatic spread. Clinical stage, serum PSA and Gleason sum score form the principal basis for therapeutic recommendations.
About 50% of cases are diagnosed at a locally advanced stage, and about 30% have bone metastases at the time of diagnosis.Men with high risk prostate cancer, including those with locally advanced disease, are at significant risk of disease progression and cancer-specific death if left untreated.
High-risk patients, including those with locally advanced disease, present two specific challenges –
* There is a need for local control, as well as
* A need to treat any microscopic metastases likely to be present but undetectable until disease progression.
Treatment options for locally advanced prostate cancer include hormone therapy, radiation therapy, radical prostatectomy (RP) or cryotherapy,alongwith adjuvant treatments where needed.
The difficulties of accurately staging locally advanced prostate cancer (LAPC) compound the frustration associated with treating these patients.One reason for avoiding RP is the concern about pre-existing lymph node invasion.Unfortunately, it is difficult to evaluate lymph node status with CT imaging, as it is insufficiently sensitive for an accurate assessment.While patients with positive lymph nodes could immediately start androgen-deprivation treatment, those with negative nodes could be monitored with serial PSA values to determine when or if they should start adjuvant/salvage therapy.
There is both overstaging as well understaging of clinical disease, so uniformly excluding patients from surgery (RP) on the basis of clinical staging may not be appropriate.One important advantage of RP – provides the true pathological stage of a patient’s primary cancer, as well as evaluating possible lymph node involvement.
Many men with clinical stage T3 disease have regional spread and may not benefit from prostatectomy; however, select patients (e.g., lower volume disease) may benefit as local control may be achieved in most, and complete cancer excision is possible in some men.
PSA value and the % of positive prostate biopsies may be helpful in selecting men with high grade prostate cancer most likely to benefit from RP.
Biochemical progression that is rise in serum PSA usually done every three monthly on follow-up, after radical prostatectomy in LAPC is difficult to assess, given the frequent use of adjuvant therapy (e.g., radiation or Androgen Deprivation).Without the use of secondary treatment, 5-year biochemical relapse is higher than 60%.With variable use of adjuvant therapy, 5- and 10-year biochemical progression was observed in 42% to 49% and 59% to 62%, respectively. The impact of adjuvant therapy may be minimal with respect to clinical progression (i.e., biopsy-proven local recurrence or objective distant metastasis) after radical prostatectomy. Rates of clinical progression at 5, 10, and 15 years are 12% to 45%, 39% to 49%, and 50% to 71%, respectively.
Radical prostatectomy alone can result in cancer-free survival in at least half of men at 8 to 10 years despite clinically advanced disease.
There is some benefit of early androgen deprivation (AD) after radical prostatectomy in high-risk men with locoregional disease spread.PSA follow-up and hormonal treatment in the case of an increase in PSA level is an acceptable option in selected cases.
Three trials have established the benefit of adjuvant radiotherapy following prostatectomy where adverse pathological features exist (margin positive or seminal vesicle positive). Adjuvant external beam radiotherapy (within 6 months of surgery) reduces the risk of biochemical failure and locoregional failure and delays or reduces the need for androgen deprivation therapy.
(The author is presently serving as consultant in GMC, Jammu)
Trending Now
E-Paper