LONDON, Jan 15: When Frederick Banting’s phone rang one morning in October 1923, it was the call that every scientist must dream of receiving.
On the other end of the line, an excited friend asked Banting if he had seen the morning newspapers. When Banting said no, his friend broke the news himself. Banting had just been awarded the Nobel prize for his discovery of insulin.
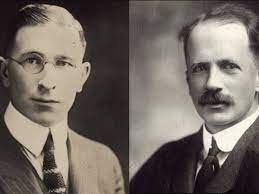
Banting told his friend to “go to hell” and slammed the receiver down. Then he went out and bought the morning paper. Sure enough, there in the headlines he saw in black and white that his worst fears had come true: he had indeed been awarded the Nobel – but so too had his boss, John Macleod, professor of physiology at the University of Toronto.
This is a tale of monstrous egos, toxic career rivalries and injustices. But of course, there is another character in this drama: diabetes itself.
According to a recent World Health Organization report, about 9 million people with type 1 diabetes are alive today thanks to insulin. I’m one of them, and it was my own shock diagnosis with this condition, just over ten years ago, that first led me to investigate the discovery of insulin – the drug that I would be injecting several times a day for the rest of my life.
‘The pissing evil’
Diabetes derives its name from the ancient Greek word for “to flow” – a reference to one of its most common symptoms and for which the 17th-century English doctor Thomas Willis (1625-75) gave it the far more memorable name of “the pissing evil”. But frequent trips to the toilet were the least of a patient’s worries.
Before the discovery of insulin, a diagnosis of type 1 diabetes meant certain death. Unable to metabolise sugar from carbohydrates in their diet, patients became weak and emaciated until, due to the production of toxic compounds known as ketones, they slipped into a coma and died.
Even at the start of the 20th century, there was little that could be done for patients with this condition, other than to put them on a starvation diet that might at best delay the inevitable.
Little wonder then that doctors were stunned at the discovery of a hormone that could return the elevated sugars in diabetic patients to healthy levels and even bring them out of a coma. And since it was made by small patches of islet-like tissues in the pancreas, this substance was given the name “insulin”, derived from the Latin for “island”.
When the eminent American diabetes doctor Elliott Joslin first used insulin to treat his patients in early 1922, he was so stunned by its power that he likened it to the “Vision of Ezekiel”, the Old Testament prophet who is said to have seen a valley of dry bones rise up, be clothed in flesh and restored to life.
Joslin’s colleague Walter Campbell was equally impressed, but much less poetic. He described the crude pancreatic extracts as “thick brown muck”.
And although the thick brown muck was saving lives, it very quickly became apparent that it could also take them. If injected in the wrong dose, it would cause a patient’s blood sugar levels to crash, sending them into hypoglycaemic shock and the possibility of a fatal coma.
For the newspapers, however, insulin was hailed as a miracle. And accolades quickly began to flood in for its discoverer. Banting received a letter from Canadian prime minister Mackenzie King granting him a lifetime pension from the government of Canada; he was invited to open the Canadian Exhibition (an honour reserved for “a distinguished Canadian or British citizen”) and was even summoned for an audience at Buckingham Palace with King George V. Then came the Nobel prize.
Why so angry?
But why was Banting so furious? As far as he was concerned, having to share the award with Macleod was not just a travesty, but an insult. He thought that Macleod had no right whatsoever to have any claim on the discovery of insulin, as an entry from a journal written in 1940 makes abundantly clear:
Macleod on the other hand was never to be trusted. He was the most selfish man I have ever known. He sought at every possible opportunity to advance himself. If you told Macleod anything in the morning it was in print or in a lecture in his name by evening … He was unscrupulous and would steal an idea or credit for work from any possible source.
And yet, had it not been for Macleod, Banting might never have been awarded the prize in the first place and would probably have remained a struggling GP in provincial Ontario.
After his return to Canada from the western front as a wounded war hero, Banting had found his career going rapidly downhill. Having trained as a doctor, he had hoped to establish a private medical practice.
But such hopes seemed to be rapidly evaporating, and he found himself cooking his meals over a Bunsen burner, writing prescriptions for baby feed and unable even to afford a trip to the cinema. Hopes of an alternative career as a landscape painter were quickly shot down in flames when his creative efforts were met with scorn by a local dealer. In every direction he looked, Banting saw a hostile world.
This also proved to be the case in his first meeting with Macleod. Banting had approached him with what he believed to be a novel approach for isolating the much sought after anti-diabetic hormone made by the pancreas that might at last tame diabetes.
But instead of being greeted with unfettered enthusiasm, Banting recalled that Macleod listened for a while and then began reading some letters on his desk.
It wasn’t that Macleod lacked enthusiasm. Rather, he was simply concerned that although Banting had the inspiration for the work, he lacked the specialist surgical skills to carry it out. But he nevertheless gave Banting the benefit of the doubt and arranged for him to begin work with Charles Best, a final year honours student.
Their partnership has since been described as “a historic collaboration” – although, as Banting later recalled, it did not get off to the best start. For when he found some serious discrepancies in some of Best’s initial data, he laid down the law in no uncertain terms:
“I was waiting for him, and on sight gave him a severe talking to. He thought that he was both God’s and Macleod’s appointed, but when [I] was finished with him he was not sure … We understood each other much better after this encounter.
With these teething troubles sorted, Banting and Best sweated away in the laboratory throughout the summer of 1921, making pancreatic extracts and testing their effects on the blood sugar levels of diabetic dogs. Banting may have been abrasive towards Best, but for his lab dogs, he had nothing but love and fondness:
I shall never forget that dog as long as I shall live. I have seen patients die and I have never shed a tear. But when that dog died I wanted to be alone for the tears would fall despite anything I could do.
With Macleod away in Europe for the summer, Banting wrote in great excitement to tell him about their latest results. But his response came as a disappointment.
Macleod gently pointed out that some of the experimental results were inconsistent and lacked appropriate controls. And when, on his return at the end of the summer, Macleod informed Banting that the University of Toronto could not agree to a list of his demands for more lab space and resources, Banting stormed out of the room raging: “I’ll show that little son of a bitch that he is not the University of Toronto,” and threatening to take his work elsewhere.
By the end of 1921, things had got worse. Macleod felt it was now time for Banting and Best to present their work in public at a formal scientific conference. But when Banting rose to address the American Physiological Society at the University of Yale that December, the prestige of the audience took its toll on his nerves. His presentation was a disaster. He later wrote:
“When I was called upon to present our work I became almost paralysed. I could not remember nor could I think. I had never spoken to an audience of this kind before – I was overawed. I did not present it well.
Desperate to snatch victory from the jaws of defeat, Macleod stepped in, took over and finished the presentation. For Banting, this was a brazen coup by Macleod to rob him of the credit for having discovered insulin – and to rub salt into the wound, it had been done in front of the most eminent doctors in the field. It confirmed Banting’s growing suspicions that insulin was slipping from his grasp – and he desperately needed to reassert his authority over the discovery.
An opportunity to do just that came in January 1922. By the time that 14-year-old Leonard Thompson’s father brought him into Toronto General Hospital, the boy was at death’s door from type 1 diabetes.
When this work was first published, Banting described how the boy’s condition had left him “poorly nourished, pale, weight 65lbs, hair falling out, odour of acetone on his breath … appeared dull, talked rather slowly, quite willing to lie about all day”. One senior medical student gave a blunt and grim prognosis: “All of us knew that he was doomed.”
Black and white portrait of a boy in a suit.
The first insulin patient, Leonard Thompson. Insulin Collection, University of Toronto.
On the afternoon of January 11, 1922, Thompson was injected with 15cc of pancreatic extract that had been prepared by Best. Hopes were high, but the effect was disappointing.
Despite causing a 25 per cent drop in Leonard’s blood sugar levels, he continued to produce ketones – a sure sign that the extract had only limited anti-diabetic effect.
(PTI)
Trending Now
E-Paper