Dr Dharma Choudhary
In recent years, there have been dramatic breakthroughs in the field of haematology and stem cell transplant, the latest being treatment through haploidentical transplantation technique that eliminates the wait time for the ones in immediate need of bone marrow transplants.
We spend much time of our lives waiting; be it in long queues, for a call back, and sometimes even for a lifeline! There are millions of people waiting desperately for lifesaving organs and bone marrow. Sadly, many die in wait to get perfectly matched donors, even for a bone marrow transplant (BMT).
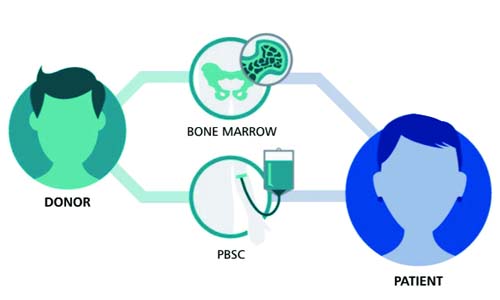
For a better understanding, bone marrow transplant is recommended in case of incurable or possible fatal blood disorders such as Acute Leukemia, Multiple Myeloma, Aplastic Anemia and Thalassaemia Major, which cannot be cured using conventional therapy, such as Chemotherapy and Radiotherapy. And for a lay reader to understand, bone marrow is the soft, fatty tissue inside our bones which produces blood cells. Stem cells are immature cells in the bone marrow that gives rise to all of our different blood cells. Now, in a typical bone marrow transplant, damaged or destroyed bone marrow is replaced with the healthy bone marrow stem cells but the major limiting factor was the availability of a suitably matched related donor. Although this limitation is partly overcome by voluntary unrelated donors available through various registries however, such representations are very less.
But with advancement in medical sciences, there is a new procedure called “haploidentical transplantation ” that virtually eliminates the waiting period for people who need bone marrow transplants on urgent basis. Through this procedure, if a donor’s tissues are only half identical with a patient’s, yet it works just as well as a complete match and the donor in this case may be the recipient’s parent, sibling, child or a family member.
Earlier people with leukemia and lymphoma used to wait endlessly for a bone marrow transplant until they could find a complete match among family members or from donors outside. With the result, as they waited, their cancer progressed, and most of them died.
Until then half-matched, or haploidentical marrow transplants, were considered impossible because of high rate of immune system rejection, slow recovery and a substantial risk of treatment-related mortality. But better knowledge, significant improvement in immunosuppressive drugs and improved techniques of T cell depletion has lead to sea change in the success of haploidentical bone marrow or blood stem cells transplant.
In this transplant program, patients are first put though few days of chemotherapy/immunotherapy or radiotherapy as per the condition of the patient before transplantation, just enough to suppress their immune system but not harm their organs. On the day of the procedure, Haploidentical donor had their stem cells collected through bone marrow.
Next, the donor stem cell is injected into the patient and 3-4 days later a high dose of immunosuppressive drugs are administered which re-boots the immune system. The medication kills off the patient’s immune cells but leaves the donated blood cells intact to create a new immune system that is more likely to be accepted by its host. Donor stem cells starts producing normal blood cells after 2-3 weeks.
The conditioning regimes which are part of the treatment have different roles to play like to eradicate malignancy and graft versus marrow effect, to eradicate remnant progenitor cells of recipient, etc. Earlier reduced-intensity conditioning were often used in older patients or patients with comorbidities in whom the toxicity associated with ablative conditioning would be unacceptable but now their role have been extended for other indications, thereby, improving overall success of BMT with limited toxicity.
Though there are certain complications like ulcer in mouth, infections, bleeding in the lungs, intestines, brain, and other areas of the body, cataract, clotting in small veins of liver, damage to the kidneys, liver, lungs, and heart, etc associated with BMT treatment, still the success rate of haploidentical transplant is essentially the same as for people who receive complete match transplants for high risk patients.
Advantages of Haploidentical Transplant:
It increases the chance of finding a donor as almost everyone has at least one haploidentical relative.
Relatives can usually be asked to donate stem cells much more quickly than unrelated volunteer donors.
Transplant can be done more timely.
Risks and failures of Haploidentical BMT
BMT from a Haploidentical family donor is associated with a risk of graft failure, recurrent infections and graft versus host disease. Thus, the success of such BMT depends on the following:
* Selection of the right Haploidentical Donor amongst the family members.
* Deliver the most suitable ‘Conditioning’ therapy to prevent Graft Failure.
* Prevent GVHD by processing the graft or using a combination of immunosuppressive drugs.
* Better anti infective prophylaxis.
(The author is Director, Bone Marrow Transplant BLK Super Speciality Hospital.)
Trending Now
E-Paper