Dr Mandeep Kaur
The human face is critical in social interactions, providing nonverbal cues regarding a person’s identity, race, sexual dimorphism, emotion, and overall health.
Whether we like it or not, judgments based on facial appearance play a powerful role in how we treat others and how we ourselves are treated. Psychologists have long known that attractive people achieve better outcomes in practically all walks of life. We have all heard, “You never get a second chance to make a first impression.” What is striking is that the judgment during the first impression is made within 1/10th of one second. Thus, disrupted facial appearance or facial deformity, may lead to psychosocial distress. It is obvious, therefore, that people with facial palsy or paralysis (FP) are immediately aware of their deformity and are extremely frightened that it will be permanent.
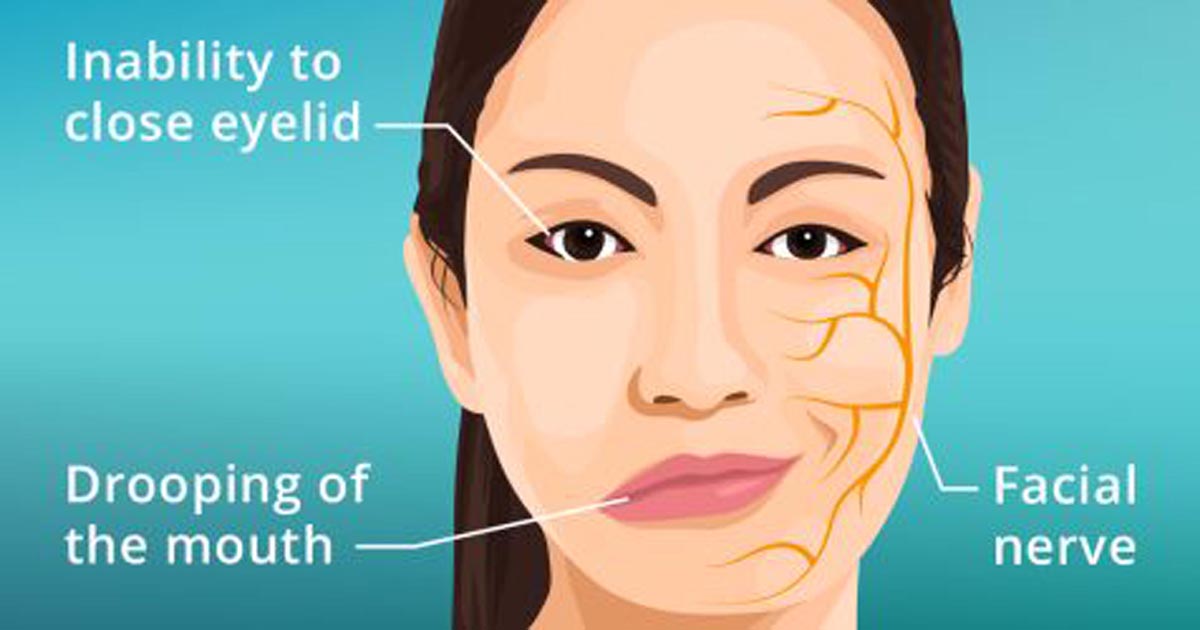
The parents of a child born with unilateral or bilateral facial palsy seek help and need qualified counselling and intervention quickly. Acquired isolated facial palsy affects 25 to 120 per 100,000, and is idiopathic, which is called Bell palsy, in 70% of cases. However, because it can be mistaken for a stroke, these patients are evaluated on an emergent basis. Moreover, whether it is idiopathic, viral, related to tumor, infection, trauma, or iatrogenic, this likewise demands comprehensive and timely intervention. Having an outline of the approach to facial palsy aids the clinician when they are confronted with a scared and worried patient and family.
How to diagnose
A thorough history may be invaluable in establishing the diagnosis thus the clinician may inquire as to the presence of otovestibular symptoms like hearing loss, hyperacusis, vertigo, imbalance, otorrhea, focal neurologic deficits (eg, diplopia, facial anesthesia), constitutional symptoms (fever, chills, fatigue, malaise, sweats, weight loss), meningitic headache, Lyme-specific symptoms like recent tick bite or exposure, erythema migrans rash, arthralgias, myalgias, low back pain, inflammatory symptoms eg, orofacial swelling or parotitis, uveitis or known autoimmune conditions and slow onset of facial weakness. Weakness in Bell palsy fully evolves over 24-72 hours. Facial symptoms vary according to the timing of presentation and degree of recovery. Other clinical signs are ocular irritation, narrowed palpebral fissure width, loss of facial symmetry at rest, collapse of the external nasal valve, oral incompetence, muscle hyperactivity, neck discomfort and facial fatigue, inability to whistle, blow cheeks, suck a straw or pronounce words, drooling of saliva from the affected side and difficulty in eating, drinking. Lack of meaningful smile also occurs in severe cases.
A thorough head and neck examination, including otoscopy and detailed cranial nerve examination, is performed. Imaging studies and MRI are done to rule out any benign and malignant tumor involving the facial nerve. Complete blood count, ESR, C-reactive protein, rheumatoid factor, antinuclear antibody, antineutrophil cytoplasmic antibody, antiphospholipid antibodies, ACE are indicated in recurrent cases, or suspected autoimmune conditions. Electroneuronography is indicated between 3 and 14 days of symptom onset in patients who present with delayed traumatic or idiopathic facial palsy.
Management
Given the breadth of therapeutic options, management of FP can be daunting. It is useful to classify patients with FP into 1 of 5 management domains, based on timing of presentation, and status of the facial nerve and facial musculature. Therapeutic strategies may include pharmaceutical agents in the form of corticosteroids, antivirals, antibiotics, corneal protective measures like daytime lubricating eye drops, Night time lubricating ointment, eyelid taping etc, physical therapy (PT) includes patient’s education and eyelid stretching, chemodenervation agents, fillers, facial yoga and a myriad of surgical procedures.
Patients with impaired facial expression due to facial paralysis experience impaired social interactions. Numerous studies have shown that such patients suffer social consequences with regards to attractiveness, affect display, depression, social withdrawal and other traits. Fortunately, reconstructive surgeries that restore the ability to express emotion can restore normalcy in these patients.
(The author is assistant Professor Dept of Oral Pathology & Microbiology Indira Gandhi Govt Dental College, Jammu)
Trending Now
E-Paper