NEW YORK, May 22: A Fitbit-like wearable device may soon help diagnose and treat asthma and other respiratory diseases, thanks to scientists who have developed a graphene- based sensor that can detect inflammation in lungs.
The sensor created by researchers at Rutgers University– New Brunswick in the US could lead to earlier detection and management of looming asthma attacks, preventing hospitalisations and deaths.
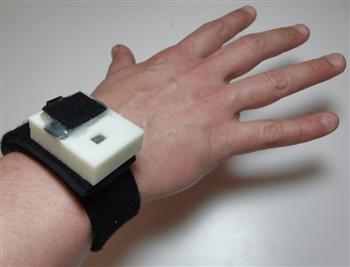
“Our vision is to develop a device that someone with asthma or another respiratory disease can wear around their neck or on their wrist and blow into it periodically to predict the onset of an asthma attack or other problems,” said Mehdi Javanmard, assistant professor at Rutgers.
The sensor paves the way for the development of devices – possibly resembling fitness trackers like the Fitbit – which people could wear and then know when and at what dosage to take their medication, researchers said.
Today’s non-invasive methods for diagnosing and monitoring asthma are limited in characterising the nature and degree of airway inflammation, and require costly, bulky equipment that patients cannot easily keep with them, they said.
Measuring biomarkers in exhaled breath condensate – tiny liquid droplets discharged during breathing – can contribute to understanding asthma at the molecular level and lead to targeted treatment and better disease management.
Researchers created miniaturised electrochemical sensors that accurately measured nitrite in exhaled breath condensate using reduced graphene oxide.
They used reduced graphene oxide as it resists corrosion, has superior electrical properties and is very accurate in detecting biomarkers.
“Nitrite level in breath condensate is a promising biomarker for inflammation in the respiratory tract. Having a rapid, easy method to measure it can help an asthmatic determine if air pollutants are affecting them so they can better manage use of medication and physical activity,” said Clifford Weisel, professor at Rutgers University-New Brunswick.
“It could also be used in a physician’s office and emergency departments to monitor the effectiveness of various anti-inflammatory drugs to optimise treatment,” Weisel said.
“Just looking at coughing, wheezing and other outward symptoms, diagnosis accuracy is often poor, so that’s why this idea of monitoring biomarkers continuously can result in a paradigm shift,” said Javanmard.
The study was published in the journal Microsystems and Nanoengineering. (Agencies)