Dr. Amresh Jamwal
Frozen Shoulder or Adhesive capsulitis or Periarthritis of shoulder is a condition characterized by pain and restriction of movements around the shoulder joint. Frozen shoulder is classified as primary or secondary. Primary Frozen shoulder occurs without an identifiable cause. Secondary Frozen shoulder occurs as a result of injury, surgery, or illness. Frozen shoulder has three distinct stages of progression:
* Painful or Freezing stage: This stage is characterized by shoulder pain. It starts gradually and progressively worsens.
* Frozen stage: Pain may reduce in this stage, although shoulder stiffness and restriction increases. Shoulder range of motion is dramatically reduced.
* Thawing stage: In this stage the motion gradually increases and the shoulder is more responsive to stretching exercises and treatment.
Each stage typically takes months to progress. The normal progression of Frozen shoulder through all three stages is between six months to two years. Without a purposeful effort to restore motion, the effects of a Frozen shoulder may become permanent.
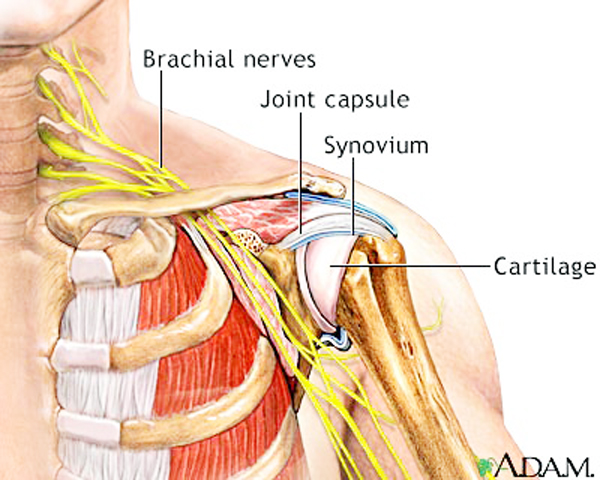
The process involves thickening and contracture of the capsule surrounding the shoulder joint. Pain due to frozen shoulder is usually dull or aching. It can be worsened with attempted motion. The pain is usually located over the outer shoulder area and sometimes the upper arm. The non dominant shoulder is usually more effected as compared to dominant shoulder. Pain may be worse at night and is provoked by lying on the effected shoulder. Motion is also limited when someone else attempts to move the shoulder for the patient.
Diagnosis of frozen shoulder is based on the history of the patient’s symptoms and physical examination. X-rays or MRI (magnetic resonance imaging) studies are sometimes used to rule out other causes of shoulder stiffness and pain such as rotator cuff tear or shoulder dislocation.
Signs and Symptoms of Frozen Shoulder:
* Decreased shoulder motion.
* Reduced arm swing while walking.
* Holding the arm in a protective manner near the body.
* Stooped rounded shoulders.
* Neck and back pain.
Frozen shoulder can develop after a shoulder is immobilized for a period of time such as in case of injury or Paralysis. Other medical problems associated with increased risk of Frozen shoulder include Cervical spondylosis, weakness of back muscles, Parkinson’s disease and cardiac disease or surgery. Attempts to prevent frozen shoulder include early motion of the shoulder after it has been injured.
Treatment of Frozen shoulder is aimed at pain control and restoration of motion. Medications for management of Frozen shoulder include Analgesics, oral steroids, and/ or non-steroidal anti-inflammatory medications. In severe cases, manipulation under anesthesia, or surgery are required to restore shoulder motion. An intensive regime of Physiotherapy is required for a couple weeks following manipulation under anesthesia to prevent new adhesions from forming following the manipulation.
Physiotherapy treatment:
Physiotherapy treatment in Frozen shoulder include techniques such as stretching, mobilization, range of motion exercises for the shoulder to increase its mobility and use of Hot packs, IFT and/or other modalities to help decrease pain. Manual mobilization of the effected shoulder should be performed by a skilled Physiotherapist. The goal of the manipulation is to manually break free restrictive adhesions and to restore motion. It bears the risk of tearing the shoulder joint capsule or causing a disruption of internal structures. The Physiotherapist manually moves the shoulder in a manner that will open the joint and place tension on the adhesions and contractures. Sometimes quick impulses are utilized to mobilize the restrictions. Frequency and duration of treatment are both dependent on the stage that the patient is in. Exercises should be done regularly 1-2 times a day. It is normal to feel aching or stretching sensations when doing the exercises. However severe and lasting pain (e.g. more than 30 minutes) is not recommended. Raising of arm forwards often improves first. Getting the hand behind the lower back appears to be the last movement to return. The movements should not feel painful although feeling of movements being stiff is normal.
Indications for treatment by Physiotherapy:
*Shoulder pain.
* Decreased range of motion.
* Impaired performance of activities of daily living.
* Decreased shoulder strength.
* Impaired function.
Contraindications / Precautions for treatment by Physiotherapy:
* Mobilization should not be given to patients with joint hyper mobility.
* Any malignancy.
* Bone disease detectable on X-ray.
* Unhealed fracture.
* Excessive pain.
* Systemic connective tissue disease.
* Joint effusion and inflammation.
* Elderly individuals with weakened connective tissue.
Some useful tips:
* If the effected shoulder causes trouble while sleeping at night, use an extra pillow. Put the pillow under your effected shoulder, and sleep on your back.
* Over-the-door pulley systems are a practical way to mobilize the shoulder in multiple planes of motion. The well arm pulls the Frozen shoulder into various stretches. Pulley exercises can be used to perform many of range of motion exercises.
* A significant number of patients with shoulder pain respond favorably to spinal manipulation so it should also be considered in cases of Frozen shoulder accompanied by reduced spinal motion.
* A common mistake of people with frozen shoulder is that they keep it still. Immobility worsens this condition. Gentle movement will help to keep the blood flowing to the shoulder.
* The application of a hot pack or warm shower prior to performing exercises and the application of an ice pack to the shoulder afterward will make the exercises more tolerable.
Remember that healing from a Frozen shoulder will take time and in some cases a lot of time. Exercises need to be done every day. You will need to push yourself out of the comfort zone to obtain healing.
(The author is a Physiotherapist)