Dr Richa Sharma, Dr Amit Basnotra
Liver is an important organ of body and liver diorders may affect the pregnant woman and her fetus.As such also pregnancy has lot of turbulent changes in body so aim is to be informed so that timely intervention can be done
How Preganancy can mask or mimic Liver diorders ?
Pregnancy can bring many changes which may mimic certain pathologies as-
* Changes in some of the tests to assess liver function
* Physical findings such as palmar erythema and spider angiomas, which may suggest liver disease, may be found during normal pregnancy
* Post delivery, there is a significant rise in serum bilirubin and transaminase, however, only 10 percent are in the abnormal range
So we should not get panic in first instance, definitely we shouldn’t ignore also and consult doctor on right time and needs Multidisciplinary approach which involves taking timely help of Gastroentrologist so that things are not missed
Diseases of the Liver
It is customary to divide liver diseases into those specifically related to pregnancy –
1.Coincidental to pregnancy -Most acute hepatic disorders complicating pregnancy are coincidental (e.g., acute viral hepatitis, drug-induced hepatic failure).
* Chronic and antedate pregnancy- pregnancy may be superimposed on chronic liver disease such as hepatitis, cirrhosis, or esophageal varices, and after liver transplantation.
* Pregnancy-induced disorders that resolve spontaneously or following delivery include hepatic dysfunction from hyperemesis gravidarum, intrahepatic cholestasis, acute fatty liver, and hepatocellular damage with severe preeclampsia.
Fatty Liver of Pregnancy
Acute liver failure during pregnancy may be caused by fulminant viral hepatitis, drug-induced hepatic toxicity, or acute fatty liver of pregnancy. The latter is also called acute fatty metamorphosis or acute yellow atrophy, and it is an uncommon complication that often has proved fatal for both mother and fetus.
Incidence – 1 in 10,000 pregnancies.
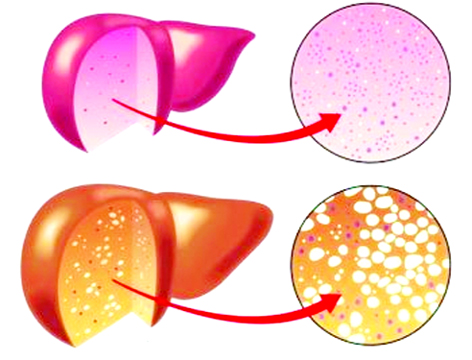
Fatty liver is characterized by accumulation of microvesicular fat that literally “crowds out” normal hepatocytic function.
Fatty liver recurring in subsequent pregnancy is uncommon, but a few cases have been described
Acute fatty liver almost always manifests late in pregnancy. Fatty liver is more common in nulliparas with 15 percent of cases there is a multifetal gestation
How the patient will present clinically ?
Symptoms usually develop over several days to weeks
Presentation Clinically can vary from- malaise, anorexia, nausea and vomiting, epigastric pain, and progressive jaundice. Some women may have persistent vomiting in late. About half of all women have hypertension, proteinuria, and edema-signs suggestive of preeclampsia. There is usually severe liver dysfunction with hypofibrinogenemia, hypoalbuminemia, hypocholesterolemia, and prolonged clotting times.
Clinical involvement is relatively minor and laboratory aberrations can be hemolysis and decreased plasma fibrinogen which needs attention. Thus, there is a spectrum of liver involvement, and hepatic failure varies in intensity, with encephalopathy as the most extensive involvement. Many milder cases may go unnoticed
Prognosis-
Although maternal mortality in the past approached 75 percent, the contemporaneous outlook is much better. Fetal mortality in the past was nearly 90 percent, but now is about 15 to 20 percent.
Spontaneous resolution usually follows delivery. Presumably because of maternal acidosis and hemoconcentration in severe cases, some fetuses are dead when the diagnosis is made. Importantly, many others tolerate labor poorly.
Nonalcoholic Fatty Liver Disease (NAFLD)
Non-alcoholic fatty liver disease (NAFLD) in pregnancy has nearly tripled over the past ten years. It increases risks for both mother and baby, including hypertensive complications of pregnancy, bleeding after delivery, and preterm birth Globally, around 25 percent of all individuals are affected with NAFLD.
NAFLD is considered the hepatic manifestation of the metabolic syndrome and is tightly linked with obesity and diabetes.
This is an increasingly recognized condition that may progress to end-stage liver disease . Although it resembles alcohol-induced liver injury, it is seen in patients without alcohol abuse. It is known by several names: fatty liver hepatitis, nonalcoholic Laënnec disease, diabetes hepatitis,alcohol-like liver disease, and nonalcoholic steatohepatitis (“NASH”).
Women with non-alcoholic fatty liver disease (NAFLD) should receive preconception counseling about increased maternal and infant risks, while pregnant mothers may benefit from evaluation by a high-risk obstetrics team
The natural history of nonalcoholic fatty liver disease has not been well defined, but is related to severity of liver damage. Some cases progress to cirrhosis. Currently, weight loss along with diabetes and dyslipidemia control are the only recommended treatment.
(The authors are senior IVF Consultant, and Senior Gastroentrologist)
Trending Now
E-Paper