LONDON: Scientists have developed three- dimensional (3D) bone tissues in the lab for the first time, which when implanted into patients will be able to repair damaged bones.
Bone is the second most grafted tissue after blood and is used in reconstructive, maxillofacial and orthopaedic surgeries.
Currently, however, surgeons can only harvest limited amounts of living bone from the patient for use in graft, and bone from other donors is likely to be rejected by the body.
Instead, surgeons must rely on inferior donor sources which contain no cells capable of regenerating bone, limiting the size of repairs they can effect.
Researchers from University of Glasgow and University of Strathclyde in the UK used technology originally developed to detect gravitational waves to generate tissue engineered bone graft.
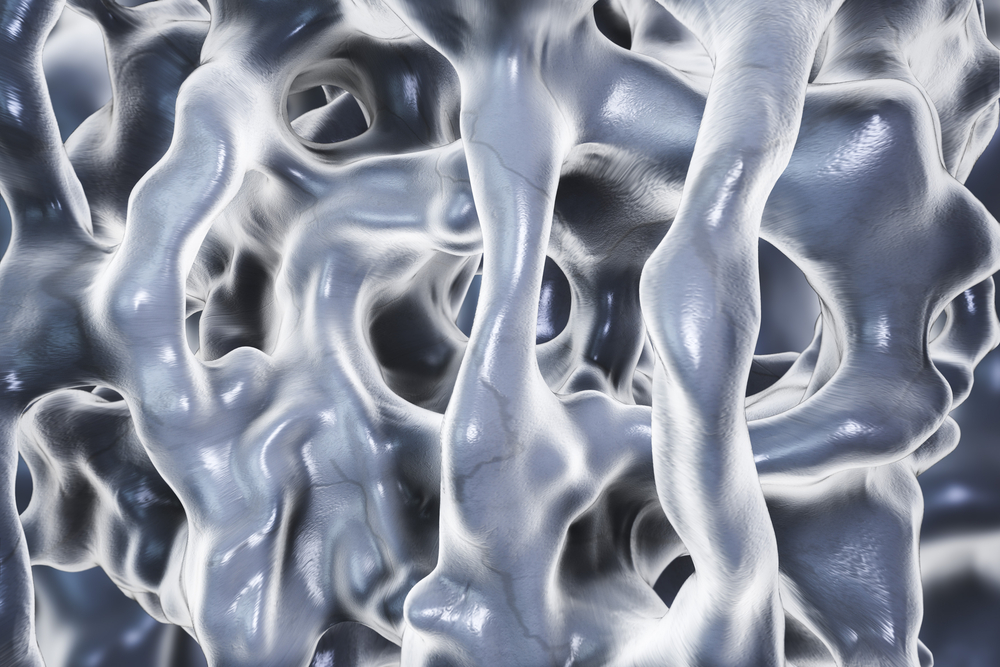
The latest development in a technique known as ‘nanokicking’ has allowed scientists to grow 3D samples of mineralised bone in the laboratory for the first time.
The researchers used measurement technology, based on the sophisticated laser interferometer systems built for gravitational wave detection of astrophysical objects, to turn mesenchymal cells taken from human donors into bone cells in three dimensions.
These 3D living bone grafts, when implanted into patients in the future, will be able to repair or replace damaged sections of bone.
Mesenchymal stem cells, which are naturally produced by the human body in bone marrow, have the potential to differentiate into a range of specialised cell types such as bone, cartilage, ligament, tendon and muscle.
Nanokicking subjects cells to ultra-precise, nanoscale vibrations while they are suspended inside collagen gels.
The process of nanokicking turns the cells in the gels into a ‘bone putty’ that has potential to be used to heal bone fractures and fill bone where there is a gap.
Using patients’ own mesenchymal cells means surgeons will be able to prevent the problem of rejection, and can bridge larger gaps in bone.
“This is an exciting step forward for nanokicking, and it takes us one step further towards making the technique available for use in medical therapies,” said Matthew Dalby, professor at the University of Glasgow.
“We have advanced the process to the point where it is readily reproducible and affordable, we will begin our first human trials around three years from now,” said Dalby.
The study is published in the journal Nature Biomedical Engineering. (AGENCIES)